Menin Related Diseases
Menin Plays a Role in Both Diabetes and Oncology
Diabetes Mellitus
Diabetes mellitus is characterized by a reduced ability to produce insulin and/or by a dysregulated response to insulin and affects nearly 34 million people in the US (Source: CDC). Diabetes is grouped into a few clinical categories based on etiology or timing of diagnosis according to the latest guidance from the American Diabetes Association. Accounting for 1.6 million diagnosed patients in the US, type 1 diabetes is due to autoimmune beta-cell destruction, usually leading to absolute insulin deficiency, including latent autoimmune diabetes of adulthood. Type 2 diabetes has been diagnosed in around 25.3 million people in the US and is due to a progressive loss of adequate beta-cell insulin secretion frequently in the presence of insulin resistance. The primary treatment goal is to achieve glycemic control by reducing HbA1c (A1c), a marker for the amount of sugar in the bloodstream, to 6.5% or lower. Glycemic control is a validated approach to delaying disease progression, which leads to significant and potentially fatal renal, cardiac, neurological, and ophthalmic comorbidities.
Loss of functional beta-cell mass is a core component of the natural history in both type 1 diabetes (mediated by autoimmune dysfunction) and type 2 diabetes (mediated by metabolic dysfunction). Beta cells are found in the pancreas and are responsible for the synthesis and secretion of insulin. Insulin is a hormone that helps the body use glucose for energy and helps control blood glucose levels. In patients with diabetes, beta cell mass and function are diminished, leading to insufficient insulin secretion and hyperglycemia. Menin is thought to act as a brake on beta cell turnover and growth, supporting the notion that inhibition of menin could lead to the regeneration of normal healthy beta cells. Knocking out the gene responsible for the creation of menin (MEN1) has been shown to result in profound glycemic control in diabetic animal models.
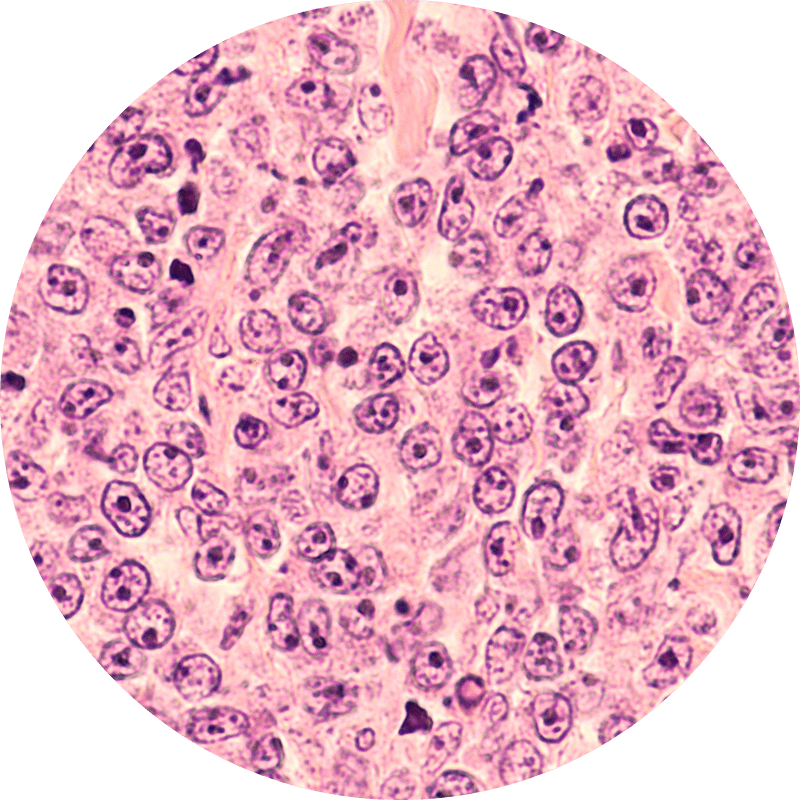
Menin dysregulation is implicated in a wide range of human pathologies, which menin inhibition can impact. Menin is a protein involved in transcriptional regulation, impacting cell-cycle control, apoptosis, and DNA damage repair. It plays a direct role in oncogenic signaling in multiple cancers. The menin complex plays a critical role in MYC-dependent oncogenic signaling, whereby menin enhances MYC-mediated transcription to promote cancer progression. The oncoprotein MYC is a master regulator of gene transcription and a potent driver of transformation. In non-transformed cells, MYC-regulated transcription is highly controlled; however, in many human cancers, MYC is dysregulated, often through constitutive and elevated MYC expression, which enables MYC to initiate and/or sustain tumor growth.
Nonclinical studies of Biomea’s covalent menin inhibitor, icovamenib, have shown sustained potent abrogation of menin-dependent oncogenic signaling and pathway control in vitro and in vivo. Icovamenib demonstrated consistent on-target inhibition with a strong anti-proliferative effect on various menin-dependent acute myeloid leukemia (AML) cell lines; diffuse large B-cell lymphoma (DLBCL) cell lines representing categories of Double/Triple Hit Lymphoma (DHL/THL) and Double Expressor Lymphoma (DEL); and multiple myeloma (MM) cell lines harboring diverse mutational backgrounds, including MYC dysregulation. Icovamenib also exhibited high potency in in-vitro KRAS-driven cancer cell models. MYC, which exerts much of its oncogenic activity through interaction with menin, is a major downstream effector of the KRAS pathway.
Acute Myeloid Leukemia
AML is the most common form of acute leukemia in adults and represents the largest number of annual leukemia deaths in the US and Europe. AML originates within the white blood cells in the bone marrow and can rapidly move to the blood and other parts of the body, including the lymph nodes, spleen, and central nervous system. Approximately 20,000 people in the US are diagnosed with AML each year, and the five-year overall survival rate in adults is roughly 29% (Source: NCI SEER Data). Among patients with relapsed/refractory disease, the need is greatest, as the overall survival is around 3 to 9 months. It is estimated that more than 45% of AML patients have menin dependent genetic drivers (MLL-r or NPM1). ALL is a less common leukemia, with around 6,000 new cases in the US each year and a higher 5-year survival rate of nearly 70% (Source: NCI SEER Data). Between 10 to 15% of adult ALL patients and 60 to 70% of pediatric ALL patients have MLL-r translocations.
Diffuse Large B-Cell Lymphoma
Diffuse Large B-cell lymphoma is an aggressive (fast-growing) non-Hodgkin lymphoma that affects B-lymphocytes, one type of white blood cell that make antibodies to fight infections and are an important part of the lymphatic system. In roughly ~30% of DLBCL patients, a cancer-causing gene, MYC, in combination with other genes, e.g. BCL2, drive the growth of the disease. These subset of DLBCL is known as Double Hit (DHL), Triple Hit (THL), or Double Expressor (DEL) lymphomas.
Multiple Myeloma
Multiple myeloma is a cancer of white blood cells, called a plasma cell, which normally help you fight infections by making antibodies that recognize and attack germs. In multiple myeloma, cancerous plasma cells accumulate in the bone marrow and crowd out healthy blood cells. In roughly 50% to 70% of MM patients, a cancer-causing gene, MYC, drives the growth of the disease. For MYC to drive MM it needs to interact with menin. MM is a cancer of plasma cells, which make antibodies (immunoglobulins) and are mainly located in the bone marrow. As cancerous cells migrate from the bone marrow, organ damage due to excess immunoglobulins in bones and blood and weakening of bones are common features. Approximately 35,000 people in the US are diagnosed with MM each year and the 5-year relative survival rate is around 56% (Source: NCI SEER Data). Among patients with relapsed or refractory disease, the need is greatest, with overall survival as low as 6 months in some patients. Additionally, it is estimated that more than 60% of MM patients have menin dependent genetic drivers (MYC addicted or driven) and that these drivers are more common in the relapsed or refractory setting.
RAS Driven Solid Tumors
RAS genes (HRAS, KRAS, and NRAS) comprise the most frequently mutated oncogene family in human cancer. With the highest RAS mutation frequencies seen with the top three causes of cancer deaths in the US (lung, colorectal, and pancreatic cancer).KRAS mutations are present in around 25% of tumors, making them one of the most common gene mutations linked to cancer. They are frequent drivers in lung, colorectal and pancreatic cancers. RAS exerts it oncogenic propertied via MYC, which is dependent on menin interaction.
Non-Small Cell Lung Cancer
NSCLC is the most common form of lung cancer, representing ~84% of all lung cancer cases or approximately 200,000 cases in the US each year (Source: NCI SEER Data). Additionally, the 5-year survival rate of NSCLC is around 25%. While lung cancer is the third most common form of cancer in the US based on incidence, lung cancer contributes to the highest number of annual cancer deaths in the US. KRAS is the most frequent oncogene in NSCLC, occurring in around 30% of patients with NSCLC.
Pancreatic Cancer
Pancreatic cancer is a relatively rare form of cancer in the US, representing approximately 60,000 cases in the US each year (Source: NCI SEER Data). Pancreatic cancer is an aggressive cancer with a five-year survival rate of around 11%, indicating that there is a large unmet need. It is rarely diagnosed early, contributing to the low survival rate. Among patients with pancreatic cancer, RAS mutations (including KRAS) occur in up to around 98% of patients.
Colorectal Cancer
CRC is the fourth most common form of cancer in the US, representing approximately 150,000 cases in the U.S. each year (Source: NCI SEER Data). These cancers start in the rectum or the colon and can be diagnosed/identified early, even potentially as noncancerous polyps. The 5-year survival rate of CRC is around 65%. Among other mutations, KRAS mutations occur in around 50% of patients with CRC.